Our scalable platform approach allows Plans to spend more time focusing on population-based outcomes and less time and money managing multiple vendors to provide a wide array of SDOH services in and around the home.
Programs that are built around a single provider relationship are limited to that one provider’s offering and fulfillment capabilities. The multi-vendor platform approach allows us to engage a full range of SDOH services, as well as the full range of fulfillment options—all backed by our regulatory and compliance technology.

Digital Wallet access to our Marketplace of flexible services simplifies the process for Plans while dramatically improving member satisfaction. This is in-home supplemental benefit delivery at scale, with support from The Helper Bees Care Concierge team.

With 15,000 members, we’ve had 67,000+ encounters.
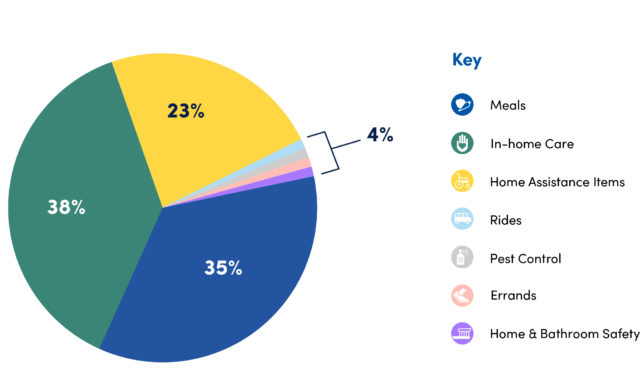
A very large and diverse network of in-home services and providers.
A technology platform that brings all those providers into a single environment to ensure compliance with state and federal requirements and provide detailed encounter reporting for plan partners.
A Care Concierge team that helps members, caregivers and plan case managers better navigate the delivery of services into the home.
Customization is a primary benefit of our platform approach. We’re not married to any single fulfillment model or caregiver type, nor are we limited by certain regulatory environments or data collection constraints. Our platform spans all regulatory models and pulls in the full range of services and fulfillment options. We can build reporting analytics that offer a single window into all data, program wide.
Our credentialing process includes an evaluation of relevant state regulatory frameworks for each service as Plan-required elements. This includes but is not limited to licensure and insurance verification, employment practice and screening policies, regular exclusion list checks, and more. With a flexible model like this, we can credential, onboard, and manage all program providers—both traditional and non-traditional—according to changing needs.
Our Care Concierge team operates in a dynamic assessment system that consistently gathers important data on a member’s social support needs at home, while auto-generating service recommendations and alert reporting back up to the Plan.
